In 2015, the Lancet Commission for Global Surgery (LCoGS) convened because surgery had yet to be considered an indivisible, indispensable part of Global Health1. The commission found that 5 billion people worldwide lack access to safe and affordable surgical care. This commission propelled surgery and anesthesia up the global priority list. The world now agrees that safe surgery and anesthesia are core components of Universal Health Coverage.
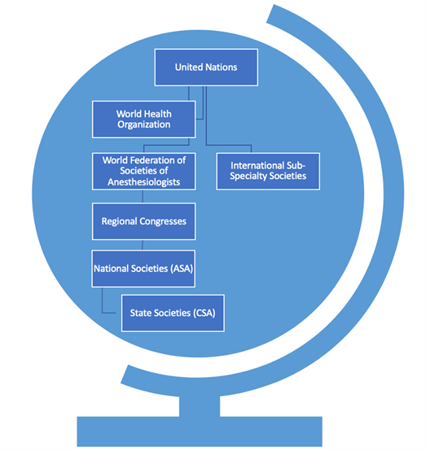
Previously deemed too expensive and resource-intensive, surgery is now accepted as cost-effective and life-preserving. The LCoGS developed core indicators, since refined to include 1) increasing the surgery, anesthesia and obstetric workforce, 2) decreasing catastrophic expenditure, 3) improving geospatial access to surgical care, 4) increasing surgical volumes, and 5) decreasing perioperative mortality2. All metrics are targeted to improve by year 20301. As Californians this may seem tangential to our daily practice, but we do fit into a global professional network (Figure 1).
Resource constraints are more and more common. Timely access to safe surgery and anesthesia is not guaranteed. This is especially apparent when healthcare systems are under strain. These challenges were evident throughout the COVID-19 pandemic; resources previously taken for granted are increasingly difficult to access. Oxygen, a World Health Organization essential medication, ran out from Los Angeles, to Mumbai, to Dar es Salaam3. Global supply chain issues continue to hinder access to our most basic medications and equipment4. Human resources are suffering. Thousands of physicians and nurses are fleeing the workforce, stressing systems experiencing increased surgical demands5. US healthcare is not cost-effective. While spending more on healthcare than other high-resourced countries, we have lower life-expectancy, a higher burden of chronic disease, and higher rates of avoidable mortality6. Environmental sustainability is a growing concern for the healthcare sector7. Concurrently, our patient populations are more diverse than ever, requiring a global-minded, culturally-informed, approach to care. Luckily, anesthesiologists are problem solvers, and this is true across the globe.
On September 7 – 11, the Rwanda Society of Anesthesiologists hosted the 8th All Africa Anesthesia Congress (AAAC) in Kigali, Rwanda. A few CSA members were fortunate enough to attend. The largest anesthesia conference on the continent, the AAAC attracts physician and non-physician providers from around the globe. The congress was also an opportunity to network with world leaders including from the World Federation of Societies of Anesthesiologists (WFSA), the World Health Organization (WHO), and the Ministry of Health, on perioperative challenges.
Anesthesia Congress (AAAC) in Kigali, Rwanda. A few CSA members were fortunate enough to attend. The largest anesthesia conference on the continent, the AAAC attracts physician and non-physician providers from around the globe. The congress was also an opportunity to network with world leaders including from the World Federation of Societies of Anesthesiologists (WFSA), the World Health Organization (WHO), and the Ministry of Health, on perioperative challenges.
Debates at the conference included how to advance our specialty while ensuring high-quality and safe patient care. There were sessions on wellness, burnout, and environmental sustainability. Most sessions evolved into high-yield discussions regarding what will and will not work in various practice settings. Participants discussed how cost-effectiveness and patient outcomes are in a constant, yet delicate balance and how best to utilize limited resources. The role of physician and non-physician anesthesia providers proves to be a universal hot topic. The learning was robust and multi-directional.
 The pandemic has proved that none of us are immune to the resource challenges faced by many of our colleagues. We have much to learn from them. No one is quicker to innovate than those forced to care for patients with too few resources. Engaging with colleagues who practice in vastly different settings creates a diversity of perspectives, strengthening our armamentarium during global challenges and in daily practice. Lessons learned from resource challenges certainly apply to those of us practicing in rural areas and in other under-resourced settings across the United States.
The pandemic has proved that none of us are immune to the resource challenges faced by many of our colleagues. We have much to learn from them. No one is quicker to innovate than those forced to care for patients with too few resources. Engaging with colleagues who practice in vastly different settings creates a diversity of perspectives, strengthening our armamentarium during global challenges and in daily practice. Lessons learned from resource challenges certainly apply to those of us practicing in rural areas and in other under-resourced settings across the United States.
Many anesthesiologists agree that engagement with professional societies such as the CSA and ASA is important for advocacy, education, networking, and ultimately improving our practice. Yet, diversity includes not just convening with our highly-resourced colleagues in North America and Europe, but also with colleagues in other parts of the world who are experts at navigating resource constraints. Learning from outside our setting prepares us for future challenges we know are coming. Strength lies in diverse perspectives and the value of collaboration is ubiquitous. As we recruit international participants to our conferences, we must ask ourselves why we would not attend theirs (Table 1).
As the pandemic wanes, many realize that greater resilience is instilled by a sense of community and greater purpose. Our global engagement is not only incentivized by the economic, practical, and political, but also the ethical and the personal. We have much to gain from a global perspective and a role to play in ensuring access to high-quality perioperative care. The experience of professional exchange and learning from others is invaluable. While striving to ensure our care is cost-effective and life-preserving and utilizing limited resources wisely, what we learn abroad improves the care of patients at home.
|
Upcoming Regional Congresses |
Date |
Location |
Frequency |
Information |
| The Asian Australasian Congress of Anaesthesiologists (AACA) | 10-13 November, 2022 | Seoul, Korea | Every 4 years | https://www.aaca2022.org/ |
| 9th All Africa Anaesthesia Congress (AAAC) | 2024 | Johannesburg, South Africa | Every 2 years | |
| Confederation of Latin American Societies of Anesthesiology (CLASA) | 14 – 17 October, 2022 | Santa Cruz, Bolivia | Every 2 years | http://www.clasa-anestesia.org/ |
| Euroanesthesia – European Society of Anesthesiology and Intensive Care (ESAIC) | 3 -5 June,
2023 |
Glasgow, Scotland | Yearly | https://www.esaic.org/events/ |
| Pan Arab Congress of Anesthesia, Intensive Care & Pain Management | 2023 | Every 2 years | http://www.pafsaco.org/ | |
| South Asian Association for Regional Cooperation | https://www.saarcaa2022.com/ | |||
| Canadian Anesthesiologists’ Society (CAS) | June 9 – 12,
2023 |
Québec City, Québec | Annual | https://www.cas.ca/en/annual-meeting/cas-annual-meeting/cas-annual-meeting |
Table 1: Upcoming Regional Conferences
References
1. Meara JG, Greenberg SLM. The Lancet Commission on Global Surgery Global surgery 2030: Evidence and solutions for achieving health, welfare and economic development. Surgery. 2015;157(5):834-835. doi:10.1016/j.surg.2015.02.009
2. Davies JI, Gelb AW, Gore-Booth J, et al. Global surgery, obstetric, and anaesthesia indicator definitions and reporting: An Utstein consensus report. PLOS Med. 2021;18(8):e1003749. doi:10.1371/journal.pmed.1003749
3. Bichnell, Rae Ellen W Lauren. In Los Angeles and Beyond, Oxygen Is the Latest Covid Bottleneck. Kais Helath News. Published online January 7, 2021. https://khn.org/news/article/in-los-angeles-and-beyond-oxygen-is-the-latest-covid-bottleneck/
4. In the Spotlight: Drug Shortages. https://www.asahq.org/advocacy-and-asapac/advocacy-topics/drug-shortages
5. Henry, Tanya Albert. Medicine’s great resignation? 1 in 5 doctors plan exit in 2 years. American Medical Association. https://www.ama-assn.org/practice-management/physician-health/medicine-s-great-resignation-1-5-doctors-plan-exit-2-years
6. OECD. Health at a Glance: United States.https://www.oecd.org/unitedstates/health-at-a-glance-united-states-EN.pdf.
7. Dzau VJ, Levine R, Barrett G, Witty A. Decarbonizing the U.S. Health Sector — A Call to Action. N Engl J Med. 2021;385(23):2117-2119. doi:10.1056/NEJMp2115675
