 Cognitive impairment after anesthesia and surgery has gained more interest in the past decade, given longer lifespans and a greater number of older adults undergoing surgical procedures. Many of these procedures are not truly elective, but rather needed to improve physical function and relieve pain. Dr. Barreto Chang and colleagues at the University of California San Francisco (UCSF) have been studying older adults undergoing spine surgeries with the goal of understanding risk factors that contribute to postsurgical complications.
Cognitive impairment after anesthesia and surgery has gained more interest in the past decade, given longer lifespans and a greater number of older adults undergoing surgical procedures. Many of these procedures are not truly elective, but rather needed to improve physical function and relieve pain. Dr. Barreto Chang and colleagues at the University of California San Francisco (UCSF) have been studying older adults undergoing spine surgeries with the goal of understanding risk factors that contribute to postsurgical complications.
One of the most common postoperative complications in older adults is postoperative delirium (POD). POD can be complex and multifactorial, and even though we have advanced our understanding, the mechanism (the how and why) is still poorly understood. Furthermore, a baseline evaluation of brain function is rarely performed before surgery, which often can lead to uncovering cognitive impairments after the surgery that may have been previously there but not diagnosed.
Dr. Barreto Chang and her colleagues from the Memory and Aging Center (MAC) at UCSF published a paper in the Journal of the American Geriatric society (JAGS) entitled “A novel approach for the detection of cognitive impairment and delirium risk on older adults undergoing spine surgery” (https://agsjournals.onlinelibrary.wiley.com/doi/10.1111/jgs.18033). They performed the Tablet-based Cognitive Assessment Tool (TabCAT) Brain Health Assessment (TabCAT-BHA), that measures associative memory, executive function and speed, language generation, and visuospatial skills with patients 65 and older undergoing spine surgeries at the UCSF Medical Center. They identified that age, baseline cognitive status, depression, and tier of surgery could be used to identify high-risk patients. The testing can be incorporated into the electronic medical record (EMR), allowing the patient’s care team access to this information.
UCSF published a paper in the Journal of the American Geriatric society (JAGS) entitled “A novel approach for the detection of cognitive impairment and delirium risk on older adults undergoing spine surgery” (https://agsjournals.onlinelibrary.wiley.com/doi/10.1111/jgs.18033). They performed the Tablet-based Cognitive Assessment Tool (TabCAT) Brain Health Assessment (TabCAT-BHA), that measures associative memory, executive function and speed, language generation, and visuospatial skills with patients 65 and older undergoing spine surgeries at the UCSF Medical Center. They identified that age, baseline cognitive status, depression, and tier of surgery could be used to identify high-risk patients. The testing can be incorporated into the electronic medical record (EMR), allowing the patient’s care team access to this information.
In a second publication this month in the Annual Review of Pharmacology and Toxicology (https://doi.org/10.1146/annurev-pharmtox-051921-112525), Dr. Barreto Chang and colleagues propose using this information in a care pathway for older adults undergoing surgery. On this pathway, older adults aged 65 or older or with preexisting cognitive impairment are administered the TabCAT-BHS prior to surgery. The results are integrated into the EMR and flagged if the patient has a high likelihood of cognitive impairment.
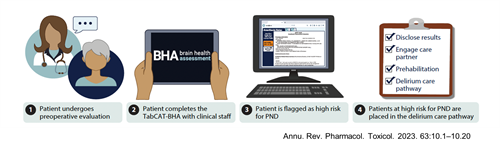
After cognitive impairment has been established, the clinical care team discloses this finding to the patient with a care partner. Lastly, prehabilitation and delirium care pathways are incorporated for patients at risk for the perioperative neurocognitive disorder (PND). The proposed pathway is in line with the American Society of Anesthesiologists’ Brain Health Initiative and the Anesthesia Patient Safety Foundation with the common goal of reducing the risk of perioperative neurocognitive disorders by targeting more individualized care to patients at high risk (https://www.asahq.org/brainhealthinitiative).
