By: Amy Chen, MD; Sehewa Mganga RN; Frank Artress, MD; Michelle Arteaga MS, MHA; Sara Strowd, MD; Cynthia Khoo, MD, PhD
The COVID-19 pandemic has dramatically impacted education including global health rotations in residency and fellowship programs. Most international travel for global anesthesia has been indefinitely postponed and many training programs transitioned to remote learning as a result of social distancing measures [1]. The Stanford Anesthesia Division of Global Health Equity had previously collaborated with Foundation for African Medicine and Education (FAME), a non-profit hospital in rural Karatu, Tanzania, where anesthesia providers were interested in incorporating peripheral nerve blocks into their practice. Regional anesthesia has been associated with reduced postoperative pain, increased patient satisfaction, as well as lower rates of morbidity and mortality compared to general anesthesia in low-and-middle income countries (LMICs) [2, 3]. However, regional anesthesia remains underutilized due to lack of infrastructure and training [4]. In lieu of an on-site visit to FAME to assist with establishment of a regional anesthesia service in 2021, a novel virtual regional anesthesia curriculum was developed in collaboration with FAME anesthesia providers. The primary objective of the remote curriculum was to introduce key regional anesthesia principles such as ultrasound anatomy, nerve block indications, and prevention of complications.
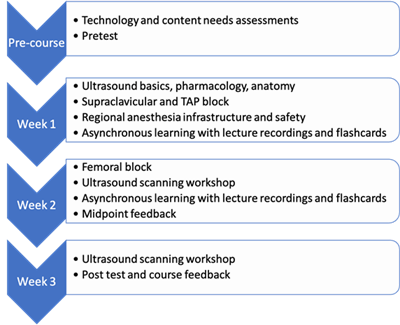
The blended learning curriculum incorporated traditional didactics, online learning, and interactive, hands-on workshops with remote supervision. A pre-course needs assessment was distributed through an online survey tool and key informant interviews were conducted. The assessments revealed that FAME facilities are well equipped for remote education with reliable internet, video conferencing space and equipment, as well as ultrasounds and other supplies. Based on participant input, the curriculum focused on ultrasound basics, nerve block procedure setup, and supraclavicular and transversus abdominis plane blocks (Figure 1). Pre-tests and post-tests of basic regional anesthesia concepts were conducted.
Using a flipped classroom approach, didactic content was distributed prior to delivering live lectures, which consisted of discussions and case-based learning. All content was recorded and made available online for review. Live lectures and ultrasound scanning workshops were conducted through video conference. Discussions and course feedback occurred daily through email and text messaging. A low-cost ballistic gel simulation phantom was used to teach ultrasound-guided needling. The phantoms were designed with 3D-printing and ballistic gel was cast into silicone shells costing twenty-fold less than commercial phantoms. The silicone shell design allows for the ballistic gel to be repeatedly recast to remove track marks and reused, which is ideal for low resource settings [5].
The final surveys indicated that the video conference lectures were valuable and considered to be as effective as in-person teaching. The anesthesia providers also indicated that the flipped classroom approach with asynchronous modes of learning such as recordings of lectures and flashcards added flexibility to their schedules. While the virtual ultrasound workshops required additional time for setup, the FAME anesthesia providers were successfully supervised as they practiced ultrasound image acquisition skills on a live model and needling skills on the ballistic gel phantom (Figure 2).
Challenges of conducting a remote curriculum in a resource-constrained setting include access to reliable internet and a video conference device. Flexibility is key. Lectures and workshops may take longer to deliver remotely, especially if a language barrier is present and nonverbal cues are lost. While ultrasound-guided regional anesthesia and other procedures have been taught remotely, formal training and supervision of nerve blocks will still require the presence of a skilled regional anesthesiologist [6]. This virtual curriculum was effective in introducing background knowledge, ultrasound image acquisition skills, and guidance on establishing a regional anesthesia service. This foundation can be built upon with in person supervision of procedures in the future.
Future educational strategies at FAME include periodic video conference lectures and utilization of the online regional anesthesia learning platform on Learnly.org created in partnership with the Stanford Anesthesia Informatics and Media (AIM) lab. On their end, the FAME anesthesia providers plan to collect a case log of surgeries amenable to regional anesthesia at their hospital and develop a system for management, documentation, and follow-up of nerve blocks. A similar remote anesthesia curriculum has already been implemented at Hue University of Medicine and Pharmacy in Vietnam and additional remote workshops are planned for the upcoming year.
Implementation of regional anesthesia in low-resource settings has great potential to reduce peri-operative morbidity and mortality as well as increase access to pain management. The current pandemic presents a unique opportunity to improve remote education, utilize modern technology, and enhance the sustainability and collaboration of global anesthesia. This curriculum demonstrates that virtual regional anesthesia education can be an interactive method of teaching fundamental knowledge, and the flipped classroom approach gives flexibility for time zone differences and clinical responsibilities. Furthermore, video conferencing is both cost and time effective for all parties involved. Remote learning allows for continuous bidirectional exchange which strengthens partnerships and may have more lasting impact than traditional global health trips. Online anesthesia education can engage a broader audience with greater continuity to achieve sustainable outcomes that improve global health equity.
References
[1] Tolu LB, Feyissa GT, Ezeh A, et al. Managing Resident Workforce and Residency Training During COVID-19 Pandemic: Scoping Review of Adaptive Approaches. Adv Med Educ Pract 2020; 11:527–35.
[2] Kessler J, Marhofer P, Hopkins PM, et al. Peripheral regional anaesthesia and outcome: Lessons learned from the last 10 years. Br. J. Anaesth. 2015;114:728–45.
[3] Ariyo P, Trelles M, Helmand R, et al. Providing anesthesia care in resource-limited settings: A 6-year analysis of anesthesia services provided at médecins sans frontières facilities. Anesthesiology. 2016;124:561–9.
[4] Ho M, Livingston P, Bould MD, et al. Barriers and facilitators to implementing a regional anesthesia service in a low-income country: a qualitative study. Pan Afr Med J 2019;32:152.
[5] Chuter B, Rodriguez S, Terajewicz A, Kaufman A, Khoo C. Design of ballistic gel phantoms for ultrasound-guided procedural training using 3D printing. Moderated session presented at ASRA 2019 World Congress on Regional Anesthesia and Pain Medicine; April 2019; Las Vegas, NV.
[6] Burckett-St.Laurent DA, Cunningham MS, Abbas S, et al. Teaching ultrasound-guided regional anesthesia remotely: a feasibility study. Acta Anaesthesiol Scand 2016;60:995–1002.
